What is a Hallux Rigidus?
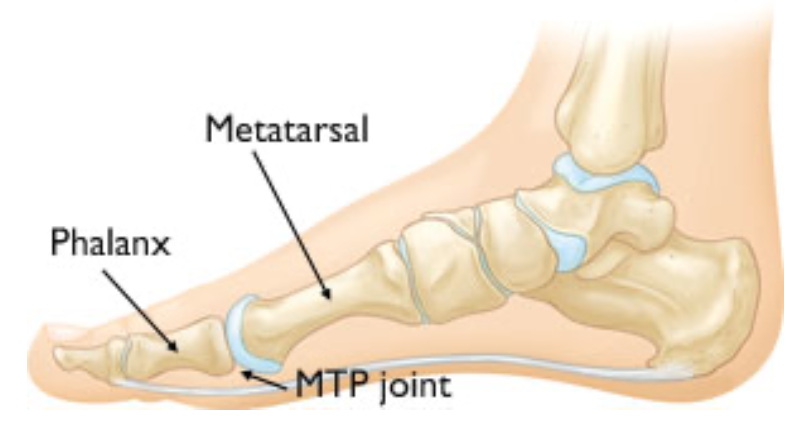
This is when the joint at the base of the big toe becomes painful and stiff as a result of arthritis. This may have been caused by an old injury, previous surgery or a long-standing bunion deformity. Pain at the joint can start to affect your daily activities and even your sleep pattern. In addition, the joint itself can develop a bony ridge due to arthritis and this can affect your ability to wear certain shoes.
Are there any alternatives to surgery?
If you decide not to proceed with surgery, you may receive advice regarding more suitable footwear. If appropriate, your surgeon may recommend a referral to the podiatrist for assessment with regard to special insoles, which may also help your symptoms.
Some patients can be suitable for a steroid injection, although this may only give short term relief.
What are my options for surgery?
If you and your surgeon feel you are ready for surgery then there are three main surgical options.
1. Try and keep the big toe joint moving. This is "conservative surgery."
2. Leave the joint stiff and stop the painful movement. This is "fusion surgery."
3. Remove the arthritic big toe joint and insert a metal and plastic replacement. This is "joint replacement surgery."
Conservative surgery
Cheilectomy of 1st MTP Joint (base of great toe)
and Moberg’s Osteotomy
What is a Cheilectomy and Moberg’s Osteotomy?
This surgery is usually undertaken as a Day Case, depending on your recovery, your general condition, home circumstances and mobility. It is best to bring an overnight bag with you just in case an overnight stay is advised. The procedure is usually performed under general anaesthesia but may be carried under local anaesthetic with sedation, spinal or epidural anaesthetic. You will have an opportunity to discuss these options with your anaesthetist and specialist before your operation.
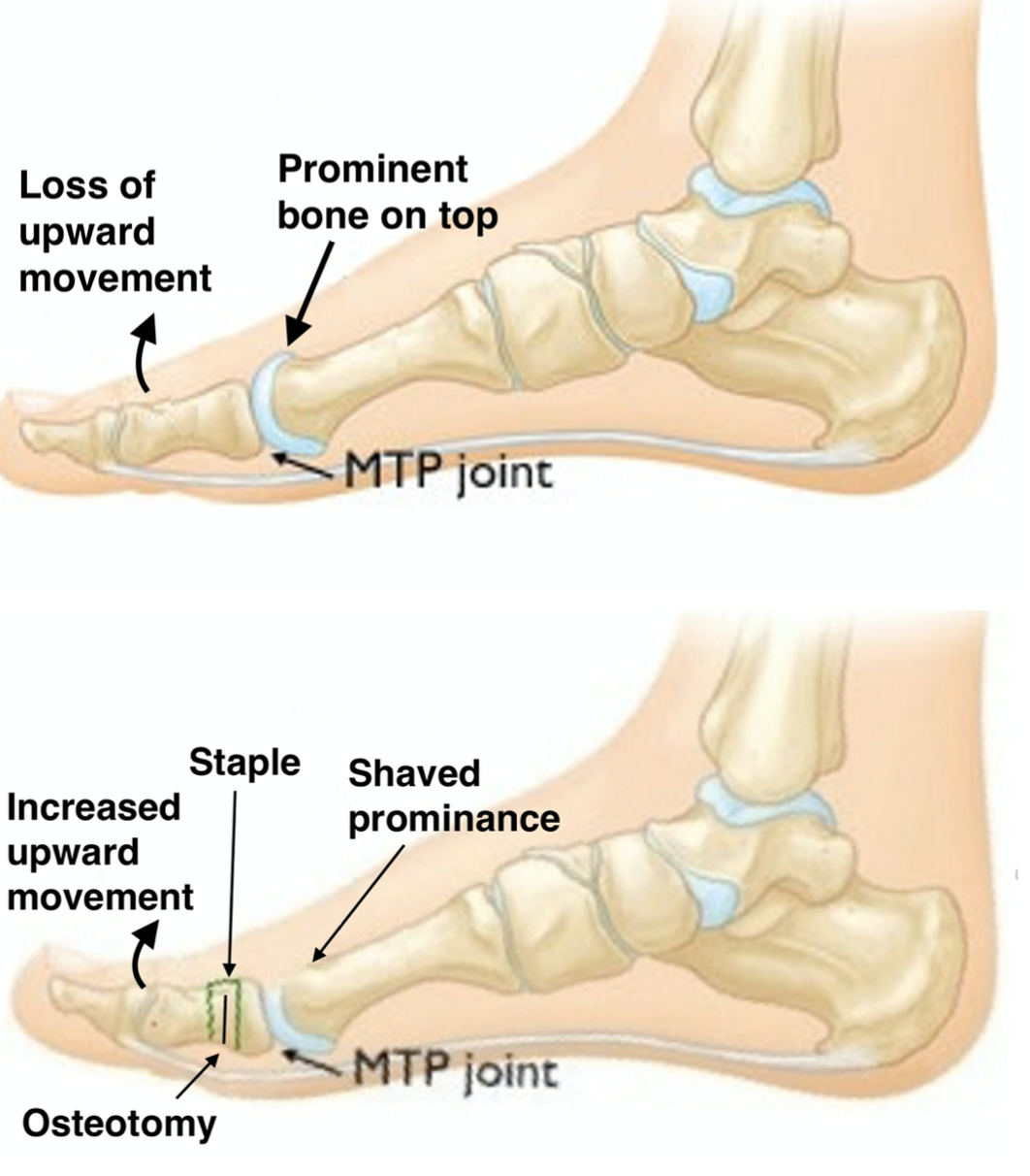
A
Cheilectomy is performed if mainly the upper part of the big toe joint is
involved. The upper part of the joint is trimmed and the joint washed out.

At the same time as a Cheilectomy, the bone in the base of your great toe may be re-aligned to make the most of the movement you have left in the joint (Moberg’s Osteotomy).
What are the benefits of having a Cheilectomy?
The aim of having a Cheilectomy is to relieve your pain and discomfort. It should allow you to wear your footwear more comfortably. Most people who have a Cheilectomy have less pain afterwards and useful movement. In about 75% of people, the improvement is long term although it can take up to a year before the full benefit is attained.
What are the benefits of having a Moberg’s Osteotomy?
The aim of having a Moberg’s osteotomy is to allow easier movement of the toe upwards, while walking. At the same time, this can be modified (Moberg/Akin Procedure) so that, in addition to the toe moving upwards, it can also be realigned to prevent it pressing on the second toe and to allow the tendons to work better, across the joint.
What are the risks of this Surgery?
Following a Cheilectomy some people can develop worsening of the arthritis and over the following years will eventually need another operation. The incision you have may be at the top or the side of your foot and this area can remain swollen for several months after surgery. In addition, if the bone has been realigned (Moberg’s osteotomy), then it may fail to heal or heal incorrectly which may leave you with pain or you may need the small metal screw or staple removing. If a nerve becomes damaged then that can lead to numbness, swelling and pain.
If you are a smoker and are about to undergo foot and ankle surgery, you are strongly advised to stop smoking for at least one week before surgery and eight weeks after your surgery. By doing this you are lessening the risk of developing a clot and you will find the healing process of the bone and wound similar to that of a non- smoker.
Do I need physiotherapy after my operation?
A physiotherapist will assist and advise you to use crutches and walk in the post-operative sandal. You will be given an outpatient appointment to see the physiotherapist to advise on mobilisation of the operated joint after your surgery
Will I Need Further Appointments in Outpatients?
You will be followed up in outpatient clinic 10 to 14 days after your surgery when your wound will be checked and any sutures removed. You will then return to follow-up clinic four weeks later when you will be re-introduced to normal footwear again, which should be flat and roomy e.g., trainers. If you have had a Moberg’s osteotomy then an X-ray will also be taken at that time.
Fusion surgery
Fusion (stiffening) of 1st MTP Joint
How is 1st MTP joint fusion carried out?
This surgery usually involves an overnight stay following your surgery, depending on your recovery, your general condition, home circumstances and mobility. The procedure is usually performed under general anaesthesia but may be carried under local anaesthetic with sedation, spinal or epidural anaesthetic. You will have an opportunity to discuss these options with your anaesthetist and specialist before your operation.
A cut is made over the joint area and the ridges of bone next to the joint and cartilage are removed. The big toe is then repositioned and then stabilised using a special plate and screws, to hold the bones together to allow healing to take place.
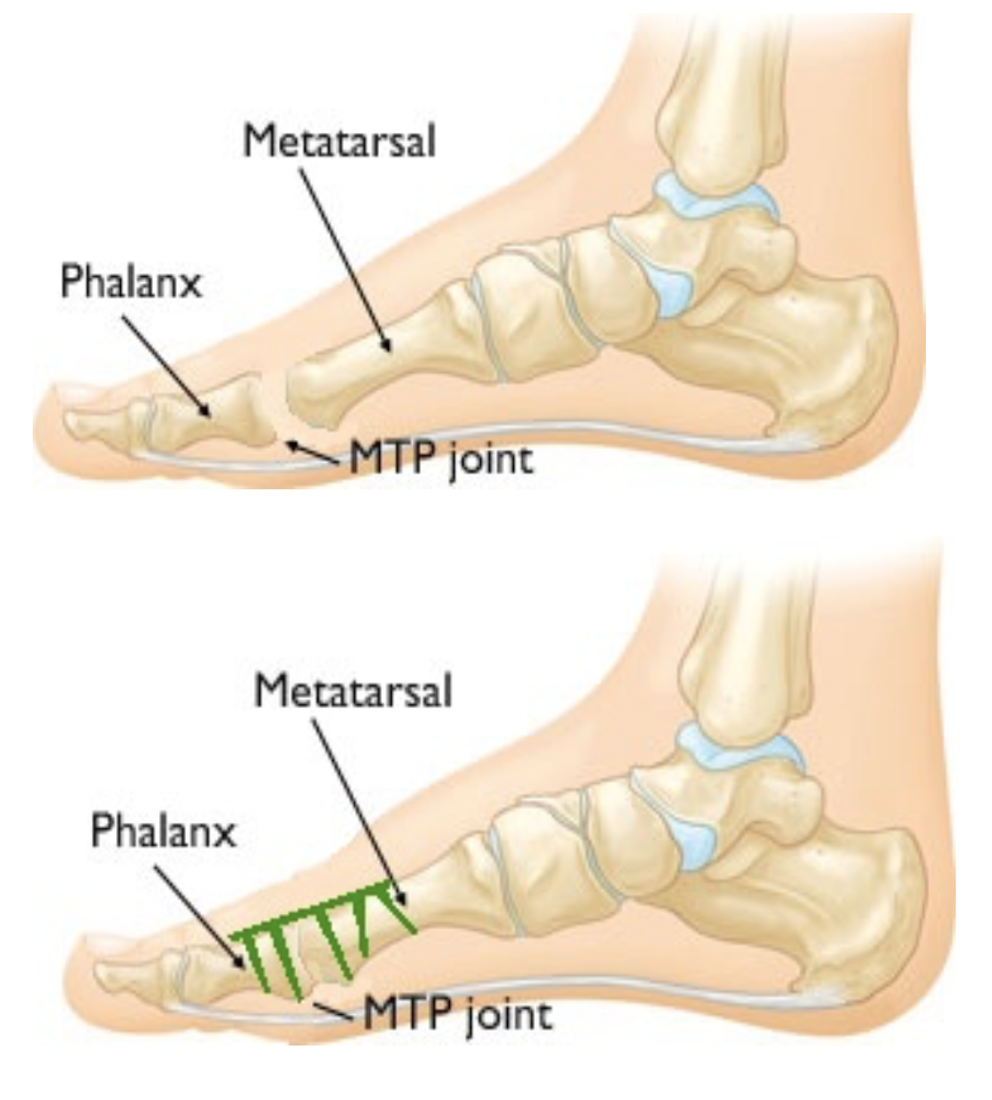
What are the benefits of having a 1st MTP joint fusion?
The aim of the procedure is to reduce pain and discomfort by stiffening the joint. This surgery should allow you to wear your footwear more comfortably.
What are the risks of having a 1st MTP joint fusion?
All surgical procedures carry risks of wound infection and delayed wound healing. There is also a risk of damage to the small nerves of your toes which may leave you with numbness or a possibly a painful scar. In addition the bone may fail to join and if you are a smoker and are about to undergo surgery, we strongly advise you to stop smoking for at least one week before surgery and for around six weeks after your surgery. By doing this you will find the healing process similar to that of a non-smoker.
Blood clot (deep vein thrombosis) is a rare complication caused by you having to be less mobile following your foot surgery. You can help to prevent this by elevating your foot when you sit (with your heel above your hip level) keeping gently mobile, wearing your stiff sandal with the aid of crutches (as instructed by the ward physiotherapist) plus carrying out frequent ankle exercises and knee bending exercises to keep your circulation moving.
Foot swelling can occur if you sit with your leg down and this can cause increased pain, bleeding and problems with wound healing.
The plate and screws usually stay in for life but very occasionally metalwork may need to be removed under general or local anaesthetic if it causes discomfort or problems, such as loosening, in the future.
Following
this surgery you will not be able to wear high heels (usually a heel height of
1 to 1![]() inches
is the maximum you are able to wear).
inches
is the maximum you are able to wear).
Do I need physiotherapy after my operation?
A physiotherapist will assist and advise you to use crutches and walk in the post-operative sandal. Physiotherapy is not usually needed after fusion surgery
Will I Need Further Appointments in Outpatients?
You will be followed up in outpatient clinic 10 to 14 days after your surgery when your wound will be checked and any sutures removed. You will then return to follow-up clinic four weeks later when you will be re-introduced to more normal footwear again, which should be flat, roomy and ideally stiff soled. An X-ray will also be taken at that time.
Joint Replacement surgery
1st MTP Joint Replacement
What is a 1st MTP joint replacement?
This is where the diseased joint surfaces are removed and a metal surface is put on the two bones adjacent to the joint with a plastic separator, allowing movement at the joint. There are many different replacements available, some replacing just one side of the joint, others acting as spacers. The one we use is the Rotoglide which replaces both diseased sides of the joint allowing up and down movement and some rotation as well which helps improve how long the joint works for.

How is 1st MTP joint replacement carried out?
This surgery usually involves an overnight stay following your surgery, depending on your recovery, your general condition, home circumstances and mobility. The procedure is usually performed under general anaesthesia but may be carried under local anaesthetic with sedation, spinal or epidural anaesthetic. You will have an opportunity to discuss these options with your anaesthetist and specialist before your operation.
A cut is made over the joint area and the ridges of bone next to the joint and cartilage are removed. The new joint surfaces are then inserted into the bones and the bone grows into the implants over time.
What are the benefits of having a 1st MTP joint replacement?
The aim of the procedure is to reduce pain and discomfort and allow movement of the joint. This surgery should allow you to wear your footwear more comfortably.
What are the risks of having a 1st MTP joint replacement?
All surgical procedures carry risks of wound infection and delayed wound healing. There is also a risk of damage to the small nerves of your toes which may leave you with numbness or a possibly a painful scar. In addition the bone may fail to join onto the implant and if you are a smoker and are about to undergo surgery, we strongly advise you to stop smoking for at least one week before surgery and for around six weeks after your surgery. By doing this you will find the healing process similar to that of a non-smoker.
Blood clot (deep vein thrombosis) is a rare complication caused by you having to be less mobile following your foot surgery. You can help to prevent this by elevating your foot when you sit (with your heel above your hip level) and carefully walking, wearing your post-operative sandal with the aid of crutches (as instructed by the ward physiotherapist) plus carrying out frequent ankle exercises and knee bending exercises to keep your circulation moving.
Foot swelling can occur if you sit with your leg down and this can cause increased pain, bleeding and problems with wound healing.
The implants can loosen over time and sometimes may need to be removed. If this happens then occasionally another joint replacement can be inserted but, more often, the joint will need to be fused (stiffened) using additional bone graft taken from the edge of your pelvis.
Do I need physiotherapy after my operation?
A physiotherapist will assist and advise you to use crutches and walk in the post-operative sandal. It is most important that you get under way with special post-operative exercises before leaving hospital. The implants join onto the bone best when you weight-bear through the operated foot and the exercise programme will be provided to you to enable you to do this with confidence. The Physiotherapists will continue to monitor and advise you in the weeks and months after surgery.
Will I Need Further Appointments in Outpatients?
You will be followed up in outpatient clinic 10 to 14 days after your surgery when your wound will be checked and any sutures removed. You will then return to a follow-up clinic two weeks later when you will be re-introduced to more normal footwear again, which should be flat, roomy and flexible soled. An X-ray will also be taken at that time. You will need to be reviewed at subsequent visits and we advise repeat Xrays at 6 months, 1 year and 2 years.
Further Information and Help After Surgery
If you have any queries or concerns after your surgery, you can contact us on the telephone numbers below
Spire Liverpool Hospital OPD - 0151 733 7123
The Bone and Joint Centre - 0151 522 1860